In discussing the quadruple challenge facing virtual care, one focuses on the major factors that mar the success of virtual healthcare. As you may already be aware, virtual care is a very fantastic idea. While it may be efficient in meeting the healthcare needs of the masses, the idea can also be dead on arrival if not well implemented. Like every other idea, there are barriers that stand between virtual care and its successful implementation. These are the major challenges that hinder its smooth running.
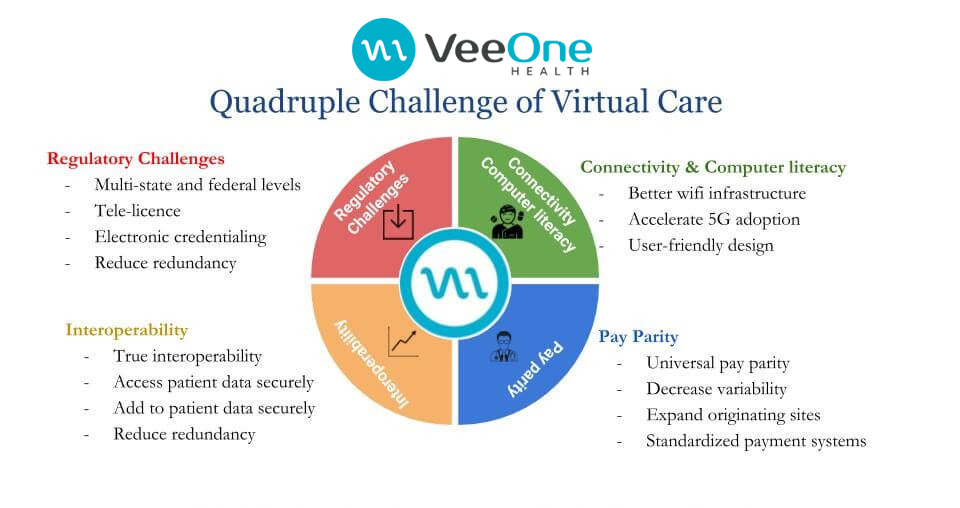
One of the biggest of these challenges is the Regulatory challenges. Here, we look at those problems that are caused by multi-state licensing. As it is with the VA system, the healthcare sector should be allowed to give virtual care to all those that are in need of adequate healthcare with a single license. Also, there are a lot of redundant credentials in the healthcare system which is not ideal. Individual health systems are often required to present different credentials for all the hospitals that are under them. This could be simplified by coming up with a more efficient way of credentialing. According to an FSMB document, there are only 12 states with special purpose license for telemedicine. Ideally, this should either be spread through all states or states should be given the room to administer virtual care without a need for different licenses.
The second big issue lies with Interoperability which is the health system’s ability to get patient’s data from different sources or different EMRs. Sadly, this is not in practice till date although ONC has been making efforts to bring this to life. If successful, it will have a lot of impact on telehealth as it will reduce the number of testing and transfers which are not very cost effective as much as they are not really good for patients. With continued efforts from the ONC, there should be a notable amount of success by 2021 to this regards.
Sadly, Connectivity and Computer Literacy remains a problem for telehealth as there remains a dearth infrastructure in healthcare institutions. There is a noticeable deficiency of strong Wi-Fi connections in most of these places. This automatically brings a halt to the success of telehealth. In the same light, there is no adequate broadband access in most homes. While the idea of 5G may be exciting, it is not likely to happen anytime soon so there is a desperate need to fix connection problems in health institutions. There should also be user friendly designs for children and aged patients. A cue should be taken from the producers of iPhone as user experience is very important to both patients and healthcare service providers.
All the while improving Provider Satisfaction. We physicians love to take care of the patient and not the paperwork. We are empowered and liberalized when we have more tools and avenues to take care of the patient. Telehealth does just that. Which indirectly decreases cost by increased iteration, decreased turnover and decreased moral injury.
Pay Parity continues to hinder the possibility of mass adoption of telehealth. So far, California remains the only state practicing true pay parity. Ideally, payment to healthcare givers should be at the same rate whether they are administering care virtually or in person, but most people do not belong to this school of thought. The public needs to understand that telehealth is a viable option to ensure that care reaches patients on time as it does not abolish the need for physical presence in ERs. If there is a need for a patient to be physically present, he/she will be asked to do so. Finally, there should be a reduced variability within states while originating sites will be made readily available, as well as a standardized payment system.
Thanks for your time! J.
Junaid Kalia MD – Telehealth, Telemedicine mHealth Strategist, Consulting & Implementation Specialist – Artificial Intelligence in Healthcare advocate & Speaker.